I love proverbs and adages, for me they encapsulate our collected knowledge to some useful sound bites. I love this one from Lao Tzu: The journey of a thousand miles begins with one step. It’s much older than that phrasing, as seen above, and for me it ties in with the idea you cannot judge a person’s actions until you walk a mile in their shoes. Everyone’s journey is unique, at times it’s easier and at others, it is so much harder.
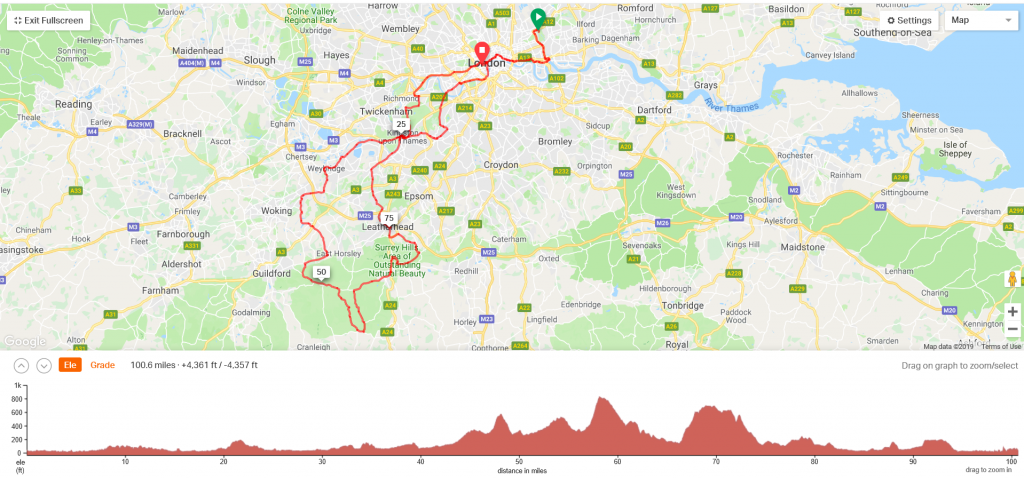
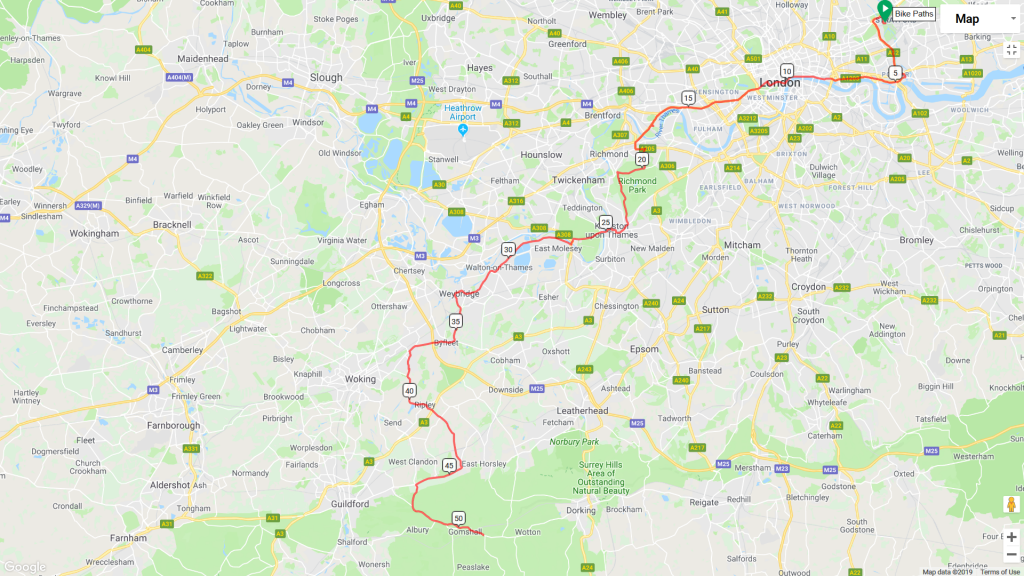
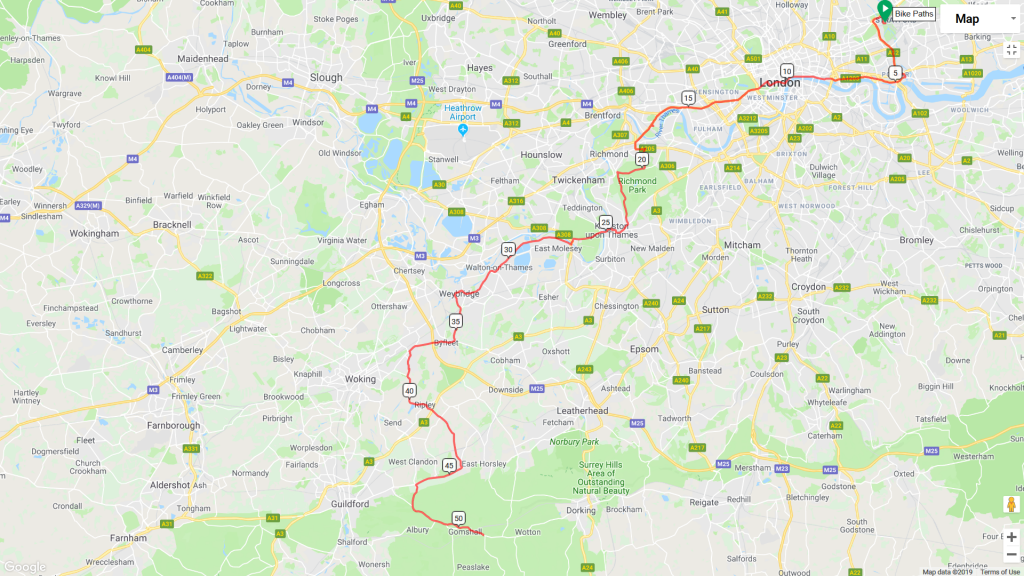
On Sunday 4th August 2019, at 5:32am my husband and I drove to Stratford and I worked out where I needed to be to participate in the Prudential Ride 100, a cycle journey around London and Surrey (not the easiest thing to do if you weren’t in the first “wave of riders”).
The 100 mile route
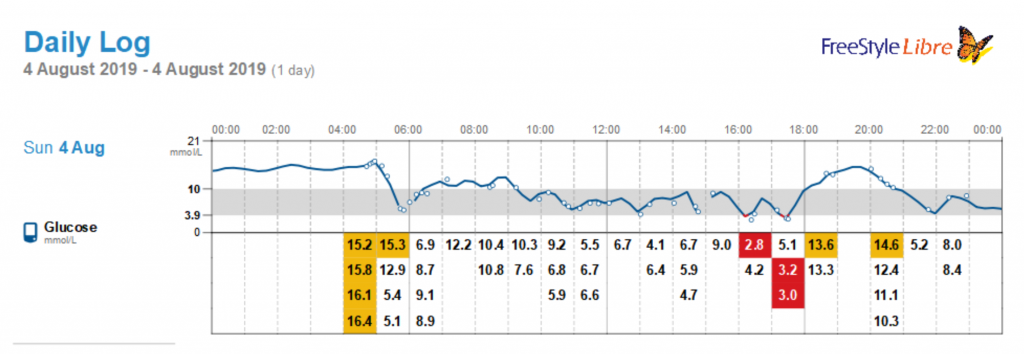
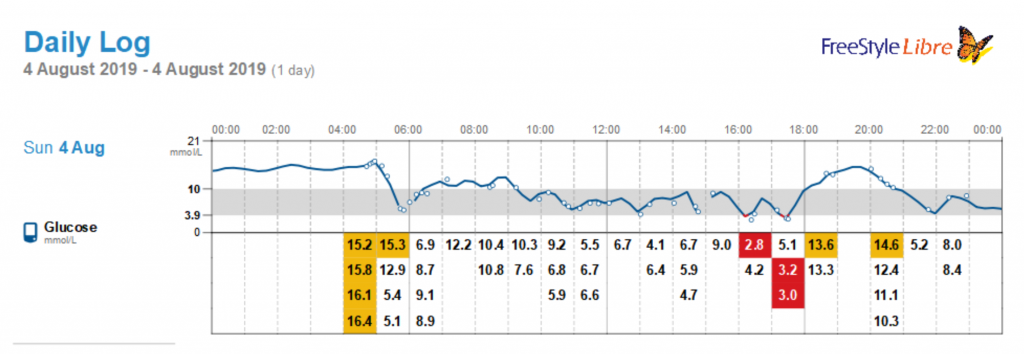
Of course, being type 1, my day didn’t start there. I woke up a bit earlier than planned (4:35 instead of 4:50), knowing that my blood sugar was high even before I reached for my flash glucose reader. Instead of following all the advice for carb loading before the start of the long ride, I was busily trying to drag my blood sugar down. After 30 mins of trying, I gave up and inserted a second new cannula and packed a breakfast.
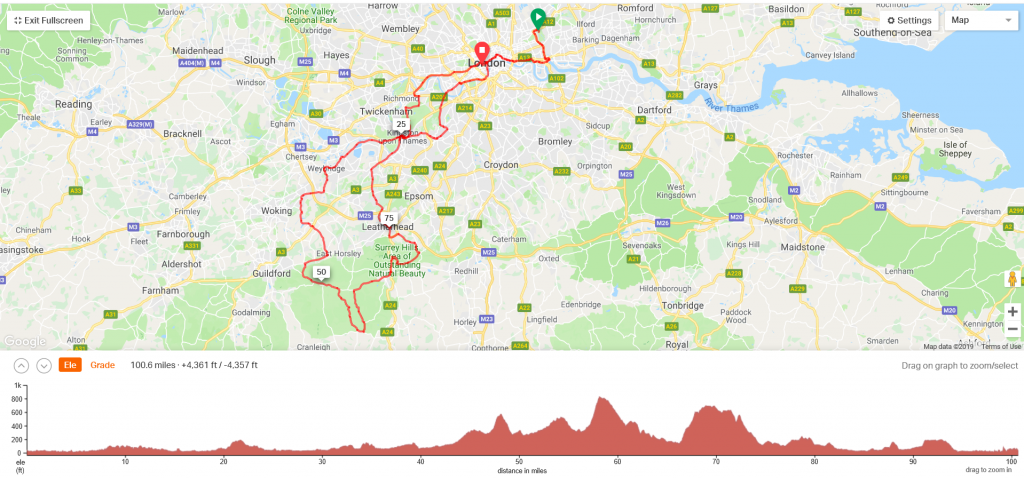
My ride in numbers
Experience had had us loading the car the night before, so armed with the consumables for the day, we headed south. I had breakfast at 5:55 as we were approaching Colchester on the A12.
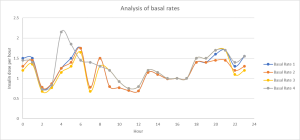
The approach I took to lower my blood glucose and ensure I could do the ride at 8:32am worked, and though I was a little high before I actually started riding the 100 miles, it was close enough with my programmed basal – basal rate 4 was the plan for that day.
Basically, normal basal up to 8am, then for an hour, up to 120% of what I normally have, then drop from 9am to 80%. That would cope with the initial push, where I dump some of my glycogen stores from my muscles and then my blood sugar starts to naturally drop.
After that first hour, I set a timer on my fitbit and every 45 minutes had a torq gel: 28.5g of available, easily digested glucose.

Torq gels
After the really steep hills, I had one at the top too and reset the timer. I’d worked out, for my estimated 8 hour ride, 10 should be plenty, but I ended up carrying 12 just in case. That was not the right number as we’ll see later.
As can be seen from my FreeStyle Libre graph, you can see when those gels were taken, every little rise in blood sugar. A rise then a dip, a rise… You can see there are some gaps in the graph: I love the Libre but it does have difficulties when my blood sugar is changing very rapidly.
What my phone caught
The first four hours dropped by, nice and easy even though I was setting a good pace. Then my phone’s battery died. Thankfully, I had my Libre’s reader with me, but my husband had headed off to catch up with some friends as 8+ hours is a long time to kill. Basically, this was noise, we were meeting up at the JDRF picnic at the end of the ride, so everything was going to be fine!
In 3hours 55minutes of moving time, I had covered 51.3miles: an average of 13.1mph, which was well within my reach. I’d peaked going down hill at 28.9mph and even on the steep hills where many were getting off their bikes to walk, I was keeping on the bike and dropping down to 4mph. My phone died at 13.10 and I completed the ride at 17:10, so I kept that pace up even though it felt like it was mostly up hill at that point ?.
Lies, damn lies and statistics
Of course, that doesn’t speak about how it felt. 100miles is a long way and nobody in their right mind should do it without some prep – as a type 1, that preparation must include blood sugar management.
It was interesting how many people struggled with energy management and struggled towards the end. They were probably much fitter than me and had lighter bikes (my push bike weighs in at 30kg when I took the rear rack off).
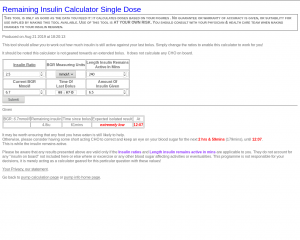
I had my gel packs (342g of CHO) and two Soreen Lunchbox loaves, which were 10.2g of CHO. That’s 352.2g of carbohydrate over an 8-hour period. I had 12 units of insulin over this period, 10.9iu as basal insulin, this rest as corrective boluses. This is not normal eating: the gels are absorbed easily; I don’t even have to chew them. They contain salts and taste nice. It meant, I could just use water during the ride, and I had nearly 6litres of water.
From 7am onwards, I didn’t eat anything else until after the ride had finished.
It wasn’t all plain sailing: there were some serious crashes, so a couple of the hills were closed off. Having been in a bad cycle accident, I hope the riders involved recover soon. I met many other crazy riders, including some raising money for Diabetes UK and JDRF. Some of them were a bit shocked I was “riding on my own” but I really wasn’t, what with the marshals, the other riders, the JDRF team and of course my husband, I was far from my own.
I had planned to have rests at the “hubs” food, drink and toilet stations. As I was one of the last “waves” to set off, I didn’t get the chance to stop at the first one (“you won’t complete the course in time to do 100miles”) which happened at the 3rd hub too. Thankfully, I was self-sufficient sugar-wise and in the Surrey hills a really nice gentleman was filling everyone’s water bottles up, which meant I didn’t need to ration my water.
Easy, peasy then!
I had a small issue with my phone – it dropped out of its holder on mile 72. Being a newish phone, I stopped, which caused my rear wheel to lock. Having gone down during a rain shower on the 18th July and cracked a rib, I released the brake and sat the bike back upright. I pulled over to the side and stopped better. Only, while I had remembered that I had a proper cleat pedal on the left hand pedal all the times I’d stopped before, my mind was on my phone and down I went.

One cleat and one not
One cleat? What are you on about?
I am a type 1 diabetic and reasonably uncoordinated and since my accident in 2017, not that confident on a push bike.
I had bought two cleat pedals and a pair of shoes to use them, but to be honest, I toppled over a couple of times which left me a sobbing wreck. I’d said I’d ride a 100miles and cleats would help me achieve that, so I had to find an alternative way to make cleats work for me.
The answer I came up with 7 weeks ago was one cleat pedal and one non-cleat pedal. I means I look a complete wally as my shoes are odd, but I get all the advantages to wearing the cleats, especially on the hills, but a lot less time spent having to plan to come out of the cleats to stop. Only I forgot when I dropped my phone.
Thankfully, it was a topple at zero miles an hour and I was wearing full length lycra trousers, so nothing worse than bruising to my skin and pride and the case my phone was in kept it safe and sound. A very kind cyclist and the marshal I went down in front of both helped me get back on the saddle.
You did it then
I did. With hindsight, I did need one extra pack of gel, so 13 rather than 12 and hold my nerve just before 3pm so I don’t correct. That would have meant I could avoid or treat the hypo at the end, the stop and then walk just used up the last of my energy. I need to figure out my phone too, so the battery lasts the whole 8hours. I overate at the picnic, a big thank you to the JDRF support team who looked after the 103 riders for JDRF – I was one of 24 who was type 1!
Unofficially I did it in 7hours 48minutes of riding. I am waiting on confirmation from the organisers on their measurements.
Would I do it again? A bit early to say. It felt pretty good finishing and basically, I pretty much made food and insulin work for me, but it did take a long time getting there 😀
If this has inspired you, I will put down all my training and approach down for other type 1s to do this themselves. Plus there’s always the place to sponsor me to raise money for JDRF: https://uk.virginmoneygiving.com/SamJWatkins – JDRF fund type 1 diabetes research to improve lives and one day eradicate the condition for good. Your support makes this happen.