Scary times
If you discuss type 1 diabetes for the first time with a newbie to the area, there are two fears they discuss. Injections/wearing a pump and hypos.
Hypos have a bad press for good reasons: people do die from them, especially the young. Of course your average non-diabetic has thousands of these a year because a hypo is any time your blood sugar is below 70mg/dl or 3.9mmol/l. A non-type 1 diabetic doesn’t have to get their “insulin dose” right: they are dealing with such small doses they can self-correct with glucagon. Everything is in a roughly 10 minute cycle (depending on the person) and unless something is badly upsetting the cycle, like not having any nutrition for 3 days (but obviously having water otherwise, you’re in bigger trouble than the hypo) or certain blood pressure medication, everything works seemlessly.
As a type 1 diabetic, things are a little different. Our insulin is typically delivered into our subcutaneous tissue rather than into the stomach cavity, so our insulin works for considerably longer than 20 minutes. To save us from injecting every 10 minutes, we either where a pump or take insulin via injections. Injected insulins can last up to 48 hours, which means potentially two days before I’m at this moment, I need to have judged exactly what insulin I need.
Which is why I’m on an insulin pump, it makes my life much easier. I’ve been pumping since December 2002 and my life would need to change dramatically to go back to injections (or my idea of smart insulin, where you inject infrequently and the insulin is released according to needs as required).
Instead of a 48 hour cycle, I’m on a 4 hour cycle, which still may mean I get things wrong occasionally.
Basal
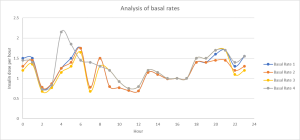
I talk a great deal about basals: this is the foundation on which my insulin replacement therapy works. If nothing else is happening, this is as solid as a lump on concrete. If I have an infection, the wrong bit of my menstrual cycle or a huge amount of stress, my basal does not automatically change to cater for that change in requirements.
This is why many are looking towards the The open source artificial pancreas system: taking readings from the CGMS I wear and controlling my pump based on those values. The promise is that if your basal is good, it should be able to stop hypos (by shutting off the delivery of insulin) and prevent highs (by turning up the basal rate). This is called closing the loop, making the pump an automated system.
Sounds great, are you doing this?
Not yet. Bear in mind if I stop my insulin for 15minutes now, it’s potentially the blood sugar result in 4 hours that is going to suffer and my basals are anything but flat. The impact when I’m using basal rate 4 of stopping my insulin between 4am and 5 am is going to be much more significant that if I do the same thing while using any of the other basals. But the same is true for basal rates 2 and 3 between 8am. Increasing my dose between 10 and noon would be impacting me just before I hit rush hour.
The impact could be huge.
That sounds very dramatic, but my Hb1Ac has always been below 8% since diagnosis. If I’m high, I generally correct so that rarely lasts more than 6 continuous hours. My lows, when I’m awake, are generally felt and dealt with – I have few lasting more than 30 minutes if I’m awake. Using my Abbott Freestyle Libre, I can now make real decisions about my overnight basal without skewing the results (that makes a huge difference). It doesn’t mean I am “not diabetic”, but it means the impact of my diabetes on my health is greatly reduced.
But it’s hard work and very stressful. I’d love to close the loop but this has to be acting quickly enough to make a difference.
But that’s not the reason for my post. I was talking about hypos. The odd hypo once in a while is normal and I am beginning to look at closing the loop on my pump with my flash glucose meter.
I’m using a tool called Glimp (on android) to do that and it classes hypos according to your blood sugar level – so anything above 3.7mmol/l is classed as mild, 3.6-2.6 is moderate and below that is severe.
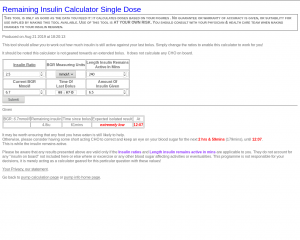
For me, that isn’t really how it works. If I have got a meal bolus wrong, say I’ve had a big meal and an hour after food my blood sugar is 6.7mmol/l (this happened once). I’d had 7.5iu to cover the big meal so I still had 4.8iu of active insulin working over the next three hours and I felt as if my blood sugar was below 2mmol/l. I treated with 40g of CHO and in three hours time, my blood sugar was 7mmol/l (I’d obviously slightly over treated).
It would have been a “severe” hypo but technically speaking, at the time it wasn’t. Indeed, if I’d been wearing a CGMS at the time, things would have looked really promising and only my experience would have told me how much trouble I was in (this was before I was using my insulin on board calculator).
I’m fairly high functioning when low, when I was in my 20s, I’d missed a drop and been happily working when I thought things aren’t right: my blood sugar measurement was 2.2mmol/l! I treated and went back to my work (I’m a computer programmer) and apart from the last couple of minutes, you wouldn’t have been able to tell. If I’d been in a meeting and talking, I’d have picked it up much sooner, but sitting at my desk, quietly plugging away, everything still worked.
Which has always made me very nervous and probably why I test as much as I do.
Lily Nichols is a non-diabetic who wore a Libre for a few days and talks about it here. The interesting thing here for me isn’t her diet but the number of “hypos” she has and the duration as seen in her graph. For us Brits, 180mg/dl is 10mmol/l and 70mg/dl is 3.9mmol/l – so she’s not going that low but the duration is surprising on the fourth day.
Her analysis is not bad although she doesn’t know what her body is doing in the background. I hear many people rave about oatmeal (Lily’s had it with honey which almost certainly accounts for the spike and her body potentially wasn’t used to have such a meal at this time, so it probably caught it unaware: do not dismiss this, the human body adapts very quickly. She runs low night: I wonder if she went out that night or was active in some other way that didn’t usually happen causing the dip. If Thanksgiving was a day she usually had a big meal, her body may not have batted an eyelid. I see this from my own results, not just from my insulin doses but how the body digests the food: My Sunday lunch, I eat 5 times the amount of carbohydrate that I normally do during the week, but rarely get high blood sugar from it. I think that’s because, that’s my normal. I do seem to “store” that energy in terms of muscle refilling as typically I do a lot of exercise on a Saturday.
Just a thought…
Posted: September 6th, 2019 under Diabetes.