Time is the enemy of us all
Yuk, depressing!
What, no! I’m not talking about aging, I’m talking about the clocks going forwards.
Losing an hours sleep, everyone whinging, boring!
I take it that you’re still out of sorts from losing that hour?
Hump…
OK, well, this time of year is hard for anyone replacing missing hormones in their body. That hour is, usually, followed by longer days and less sleep full stop. Ironically this stress on my body just makes me want to curl into a ball and fall asleep but due to high pollen counts last week, I had the added joy of antihistamines.
Whinger…
Hey. While I have managed to get 6+ hrs most nights the past couple of weeks, it has not been in continuous, uninterrupted bliss. While I’ve had a “closed loop” pump, it was allowing me to go very high “to prevent hypos” which just meant I couldn’t get to sleep in the mornings. Fun. So that’s been off for a couple of weeks now, lowering my “go to bed” values and stopping the high alarms. I am back up to > 94% in range too (the 6% out of range is typically on the low side) – and if we count what non-diabetics have their blood sugar at, more than 97% with most of the out of range values being on the high side.
Oh, that’s confusing
Even 5 years ago, the common consensus was that “normal people” had blood sugar between 4 and 8 mmol/l when ever you test them. The widespread use of continuous and flash glucose monitors shows this is not true. A fit and healthy adult typically has a range of 3.5 and 6.7 mmol/l – the 3.5mmol/l tends to self correct without any undue harm.
The ranges for type 1 diabetics tend to be a little higher, 4 and 10mmol/l, for historic reasons – insulin has a parabolic action over a number of hours when given subcutaneously. If giving large doses of long acting insulin, 4mmol/l is borderline “hypo”. Though in our non-diabetic adult, it wouldn’t cause concern as their insulin would not be released and glucagon would be given until the values raise.
My glucagon reaction is there, although it’s fighting much higher levels of insulin over a longer period, so sometimes I need to give extra glucagon infra-musculy.
Still confused!
OK, so doing this myself, most of my values are within range with peaks during meal times or having corrected a lone at 3am.
If we look at 8:47am (just after I had breakfast), my closed loop system would have shut off my basal insulin (given once every three minutes to cover my background requirements) and waited until I got back up to 6.1mmol/l, which happened due to breakfast at 9:07am. That gap at that point in the morning would mean I was then hyper (above 10am) at 11am. To counter this behaviour (as I couldn’t alter its algorithm and decision making). I had put nearly 4iu on my basal at various times fo the day.
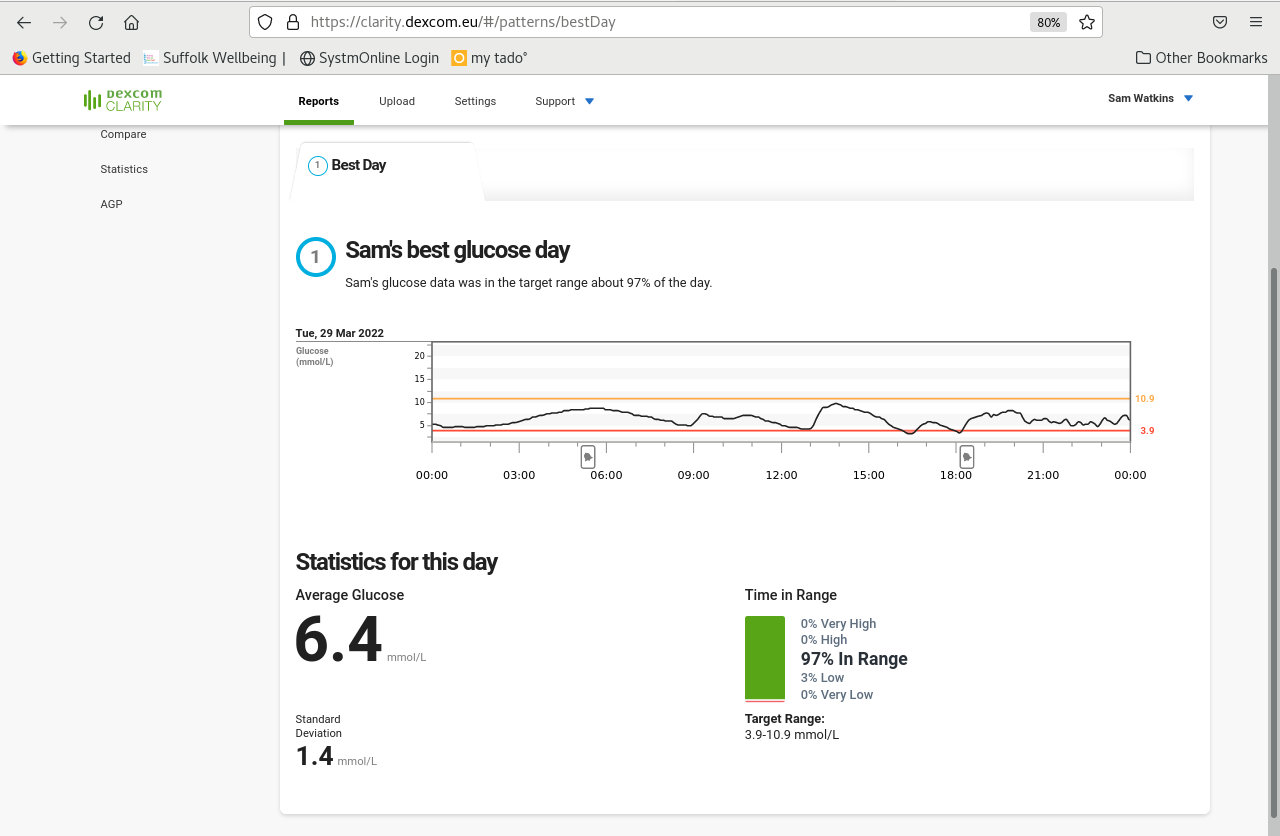
Having used the pump in open loop mode, my basal has gone from 42iu a day to 38iu and as you can see, my evening levels are pretty spot on. I had a late lunch and didn’t bolus quite on time, but that is a decent graph and an average of 6.4 – the closed loop was averaging 7.3mmol/l as an average.
The evening meal, which tends to be my main eating event of the day, was typically high using the closed loop as it was desperate to prevent a hypo and shut of my basal for up to 45 minutes after eating although you can see from the graph above that just didn’t happen.
Is man better than machine?
I think there are a few learnings:
- The basal has to be good to start with
- You cannot tune the basal with the closed loop going
- It is much more proactive stopping hypos without trusting I know what I’m doing basal wise
- I’ve set up the pump with my ratios for insulin effectiveness and carb to insulin ratios. They may be exactly what I use, but I also use the exception rule – different foods act in different ways and I balance meals effectively.
I also understand that between basal pattern shifts, things need to be a little looser on occasion.
The really irritating thing is when I’m correcting under bolusing – not giving enough insulin when eating. It assumes you’re effectively overdosing and switches off your insulin when your blood sugar is high – doh.
When I do this myself, I do a differential – I wait until my blood sugar is back to 10mmol/l and then work out if I have too much insulin on board – the amount of active insulin in play and how long that’s going to last – if it’s 30 minutes, I may just keep an eye on everything but if it’s 3iu over 3 hours, I’d tune the basal or have a little corrective carbohydrate to ensure I end up around 4.5-5 mmol/l.
It’s not the closed loop algorithms’ fault. It does not have the full picture – indeed, if I haven’t bolused, it does a reasonable job. But it is not good working out, even if I tell it I’ve had CHO, that I need insulin after 45 years of not making my own.
Posted: April 1st, 2022 under 42, Diabetes.
